Skull Base Osteomyelitis: An emerging clinical entity.
- Sampath Chandra Prasad Rao
- Apr 23, 2021
- 3 min read

What is Skull base osteomyelitis (SBO)?
Skull base osteomyelitis (SBO) is a complex and fatal clinical entity that is often misdiagnosed for malignancy. SBO is commonly a direct complication of otogenic, sinogenic, odontogenic, and rhinogenic infections. It is an infection of the temporal, sphenoid, or occipital bone that can be a challenge to diagnose because of its nonspecific symptoms, long clinical course, and radiologic findings that mimic those of other entities.
Clinical profile
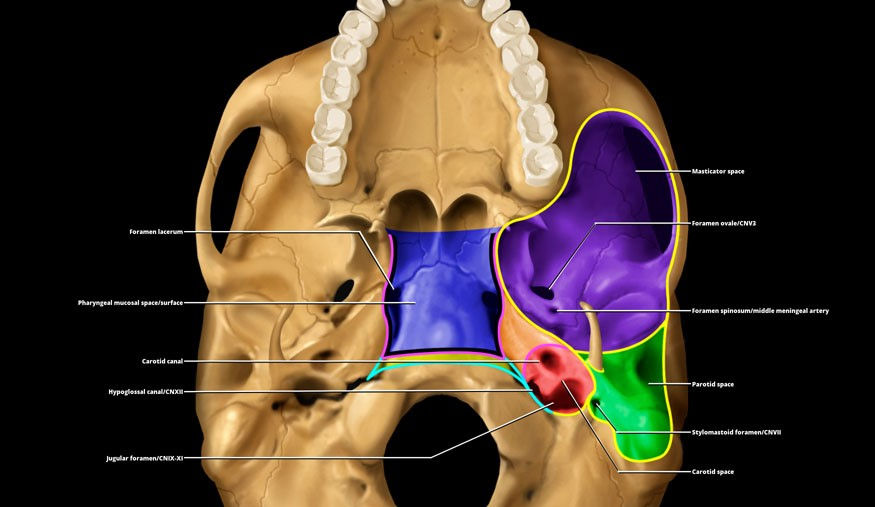
Patients with SBO frequently have nonspecific symptoms such as headache and facial pain, and therefore they exhibit a variety of clinical presentations. Most patients start with otitis externa and present with a headache, severe otalgia, facial pain, purulent otorrhea, and, in advanced cases, conductive hearing loss. In other cases, the origin might be a sinus disease, resulting in nasal congestion, rhinorrhoea, headache, and fever. Various cranial nerve palsy is also common.In general, patients usually experience lower cranial nerve palsy, because the inflammatory process is near the neural foramina. Because of its proximity to the external auditory canal at the exit of the skull base, one of the nerves that is most frequently affected is cranial nerve VII when the stylomastoid foramen or the mastoid process are involved, and this can cause facial pain and peripheral facial paralysis. This condition can be accompanied by sensorineural hearing loss when cranial nerve VIII is involved. Abducens nerve (VI) palsy can occur if the petrous apex is involved, manifesting as binocular diplopia. If the jugular foramen is affected, palsy can be present in cranial nerves IX, X, and XI and can cause a soft palate mobility disorder, unilateral vocal cord paralysis, and an inability to raise the arm above the horizontal plane, respectively. Similarly, hypoglossal canal involvement causes cranial nerve XII neuropathy, with tongue movement disorders.
Who are at risk?
Patients with SBO typically are elderly and have diabetes or are immunosuppressed.
Other diseases that alter the vascularization and oxygenation of bone predispose patients to SBO, such as small vessel disease, radiation exposure, malignancy, osteoporosis, osteopetrosis, anaemia, malnutrition, and Paget disease of the bone. Other risk factors include cardiovascular disease, renal failure, hepatic failure, obesity, smoking, extended hospital stays, and chronic pulmonary disease.
Causative pathogens
Pseudomonas aeruginosa is the most prevalent bacteria, followed by Staphylococcus aureus. Other bacteria that are seen less frequently include Staphylococcus epidermidis, Salmonella species, Proteus mirabilis, nontuberculous Mycobacterium species, Streptococcus pneumoniae, Treponema pallidum, and Klebsiella species. There is general agreement that the most frequently seen fungus is Aspergillus species, although it depends on the study.
Investigational approach
The imaging techniques used to diagnose SBO are nonenhanced and contrast-enhanced CT, enhanced MRI, and nuclear imaging. CT is the best option for evaluating bone erosion and demineralization, MRI can help delineate the anatomic location and extent of disease, and nuclear imaging is useful for confirming bone infection with high sensitivity.

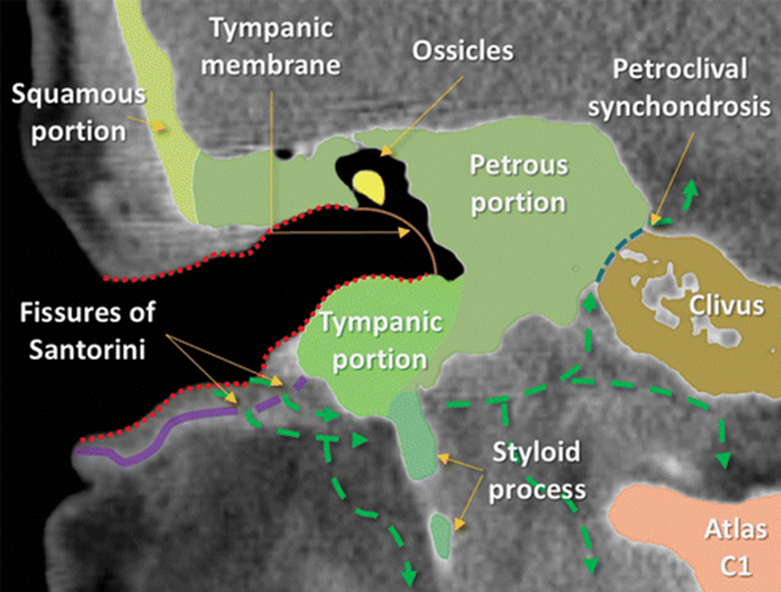
3:Coronal CT image shows the spread of infection (green arrows) in a patient with otogenic SBO of the temporal bone. SBO is usually secondary to otitis externa. From the external auditory canal, the infection reaches the temporal bone through the fissures of Santorini. The infection can spread anteroinferiorly to the parotid, masticator, or parapharyngeal spaces, medially to the carotid or perivertebral spaces, and even into the spinal canal. Intracranial spread can also occur by extension through the petroclival synchondrosis.
Management techniques
Complete resolution of the SBO cases may take several months. Since early treatment can improve mortality rates, it is paramount that the reporting radiologists and treating clinicians are aware of the cardinal diagnostic signs to improve clinical outcomes of the disease.
Given the clinical suspicion for SBO and compatible radiologic imaging, early empirical therapy with broad-spectrum intravenous antibiotics is essential. Adequate control of risk factors (such as diabetes) is also important. Intravenous antibiotics should be administered for at least 6 weeks, with subsequent oral antibacterial or antifungal therapy for 12–48 weeks.
Surgical debridement might be necessary in specific cases, including those with extensive soft-tissue involvement, severe pain despite antibiotic treatment, complications (abscess formation), or bone sequestrum, as well as refractory cases. Other management approaches for complications, such as endovascular therapy for pseudoaneurysms and anticoagulant therapy for venous sinus thrombosis, should be individualized.
Combining hyperbaric oxygen therapy can improve the treatment, given that it increases the partial pressure of oxygen, reverses tissue hypoxia, improves phagocytosis, and promotes angiogenesis and osteoneogenesis. Treatment consists of 100% oxygen administered for 90 minutes at 2.5 atmospheres of pressure 5 days a week for 1 month.
The global survival rates for SBO are approximately 90% at 18 months and 57% at 3 years. In the diabetic population, the survival rates decrease by 21%–70%. Depending on the study, the mortality rate ranges from 9.5% to 46%. The rate of neurologic sequelae is 31%–48%.
Reference
Álvarez Jáñez F, Barriga LQ, Iñigo TR, Roldán Lora F. Diagnosis of Skull Base Osteomyelitis. RadioGraphics. 2021 Jan;41(1):156-74.
Prasad SC, Prasad KC, Kumar A, Thada ND, Rao P, Chalasani S. Osteomyelitis of the temporal bone: terminology, diagnosis, and management. J Neurol Surg B Skull Base 2014;75(5):324–331. Crossref, Medline, Google Scholar












Comments